6 March 2005: Updated 15 March 2013
Contact: Stephen M.
Apatow
Founder,
Director of Research & Development
Humanitarian
Resource Institute (UN:NGO:DESA)
Humanitarian University
Consortium Graduate Studies
Center
for Medicine, Veterinary Medicine & Law
Phone:
203-668-0282
Email:
s.m.apatow@humanitarian.net
Internet:
www.humanitarian.net
H-II
OPSEC
Url:
www.H-II.org
Pathobiologics
International
Internet:
www.pathobiologics.org
Pathobiologics
International Consultancy Contact:
Antibiotic
Resistance - Enteric Disease

|
Several years back, one of my
clients had a top level dressage horse heading for Gran Prix, that
presented acute illness prior to a show in in the Western United
States. The horse was shipped to a diagnostic lab, testing
negative for salmonella upon admission, but positive during the
observation period. The horse never fully
recovered, leaving the owner/trainer devastated, with significant
expenses
associated with veterinary care.
|
In
recent years there have been important changes in antibiotic therapy in
equine
practice. There are new antibiotics available and there is more
information available on the antibiotics used in horses. Concerns over
drug residues
in food animals and antibiotic resistance has lead to the
development
of the Canadian Veterinary Medical Association's Prudent Use
Guidelines.
These guidelines stress obtaining a diagnosis and selecting
appropriate antibiotic
therapy. In practice situations, it is often difficult to submit
samples
for microbiologic culture and antibiotic susceptibility testing.
Practitioners
often choose antibiotics selection based on data from university
teaching
hospitals and veterinary diagnostic laboratories from other parts of
Canada,
the United States and even Europe. -- P. M. Dowling, "Bad Bugs, Bad Bugs, Whatcha Gonna Do?," presented at, and appears in the
Proceedings of, the 2003 Alberta Horse Breeders and Owners Conference,
11 March 2003.
Since no commercially available vaccine exists for pathogens such as Salmonella, disinfection and
other biosecurity practices must be utilized in order to prevent the
introduction or the spread of this disease. -- Animal Health Advisory:
Multi Drug Resistant Strains of Salmonella in Horses, Cornell’s College
of Veterinary Medicine, June 2004.
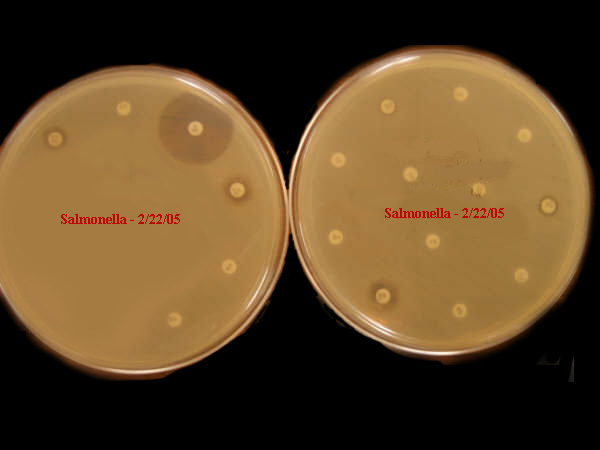
The following microbiologic culture
and antibiotic susceptibility test demonstrates the level of antibiotic resistance recently isolated at
livestock operations in the United States. Disclosure
of such
findings, by the academic community, is crucial.
|
Sensitivity: Salmonella
U.S. Test: February 2005
Embracing challenges
associated with drug resistant pathogens, water conservation
initiatives, environmental contamination, agricultural and public
health impact.
|
Antibiotic
use and resistance in food animals is as a breeding ground for
resistance genes and operons, for the accumulation of these genes on
integrons and their movement to plasmids and other accessory elements.
That is, animal use could in principle be a selective force responsible
for the assembly
of resistance gene clusters [like that postulated for the
vancomycin-resistance operons in Enterococcus or the
multiple-resistance island in Salmonella
DT104] -- Antibiotics in agriculture: When is it time to close
the barn door?," PNAS, April 30, 2002, vol. 99, no. 9, 5752-5754.
During the AAEP Convention 2004: Medicine II--Salmonella,
the question was asked: What type of impact can a salmonella
outbreak at a veterinary hospital have and what can be done to prevent
it?:
"Magdalena Dunowska, DVM, PhD, postdoctoral fellow in the veterinary
teaching hospital at Colorado State University (CSU), discussed this
issue at the 50th annual American Association of Equine Practitioners
(AAEP) Convention in Denver, Colo., Dec. 4-8, 2004. She told the group
that the James L.
Voss Veterinary Teaching Hospital at CSU was hit with salmonella
outbreaks
in 1996 and 2001. The 1996 outbreak, she said, resulted in the hospital
being closed for three months. The cost to the university for the
closure
was $500,000.
Yet the losses were greater because the $500,000 only covered expenses
of clearing the hospital of the bacteria and does not include losses
from clientele who were not allowed to bring horses to the facility."
Related
discussions:
- Methicillin-resistant Staphylococcus aureus in Horses
and Horse Personnel, 2000–2002: CDC Emerging Infectious Disease,
Vol. 11, No. 3, March 2005.
- Methicillin-resistant Staphylococcus aureus: An
emerging problem in horses?: JAVMA, 15 November 2003.
- Presence of vancomycin-resistant enterococci in farm
and pet animals: Antimicrobial Agents and Chemotherapy, Oct
1996,
2285-2287, Vol 40, No. 10.
- National
Antimicrobial Resistance Monitoring System (NARMS): A list of all publications from peer-reviewed
medical literature using NARMS data.
- Life-Threatening Infantile Diarrhea from
Fluoroquinolone-Resistant Salmonella enterica Typhimurium with
Mutations in Both gyrA and parC: CDC Emerging Infectious Diseases,
Vol. 9, No. 2, February 2003.
- Nosocomial Outbreak of Fluoroquinolone-Resistant
Salmonella Infection, NEJM, Volume 344:1572-1579, Number 21, May
24, 2001
- Co-Infection A-Fujian-H3N2 - Methicillin Resistant
Staphylococcus Aureus: VRE, MRSA, and Influenza: Emergence of
Methicillin-Resistant Staphylococcus aureus as a Cause of
Community-Acquired Pneumonia During the Influenza Season, 2003-2004.
EQUINE
ADVISORY: CORNELL
Animal Health Advisory: Multi Drug Resistant Strains
of Salmonella in Horses, Cornell’s College of Veterinary Medicine,
June 2004:
The NYS Veterinary Diagnostic Laboratory has isolated Salmonella
Group C2 from cultures submitted from 7 horses of 4 different horse
farms
in either New Jersey or Pennsylvania, in one week. They have all shown
the same profile, being resistant to most antibiotics. They awaiting
further identification of these isolates. A Salmonella Newport strain
(Group C2) was recently associated with the closing of the University
of Pennsylvania’s large animal clinic, New Bolton Center, and was also
reported to be multi-drug resistant.
Salmonellosis is generally a disorder of the gastrointestinal tract.
Stress such as surgery, transportation, hospitalization, training,
antibiotic therapy, or dietary changes
can lead to its development in the presence of infection. Symptoms are
caused by toxins produced by the Salmonella species bacteria. Signs
exhibited relate to four distinct types:
1) active carrier that appears normal
2) depression, fever, loss of appetite
3) severe case of enteritis and colitis that exhibits diarrhea and/or
colic
4) generalized septicemia that can lead to rapid death or later bone
and joint infections. Transmission to other horses is by the oral
route, entry through umbilical stump in foals less than 30 days of age,
or an
open wound.
It is unknown how and when multi-drug resistant Group C2 Salmonella
strains have emerged in the equine industry, or how widespread they
are. It is believed that extensive non-therapeutic use of antibiotics
exposes too many pathogens to levels of antibiotic which then causes
“hardy” strains to survive. At this point, the cultures received at the
lab have all been from sick foals or from the environment in which sick
animals with confirmed Salmonella cultures were housed. It is advised
that equine operations be alert to the possible spread of these
organisms. Illness can be difficult to treat, may be fatal, and the
environment, once contaminated, may be difficult to clean up. Other
livestock and companion animal species are also susceptible to
infection. Horse owners and caretakers should be alert to equine
illnesses involving fever, diarrhea and colic, especially in foals,
and call their veterinarian promptly. Fecal or blood culture (sick
foals,
especially) samples from all horses with such symptoms should be
promptly
submitted to the New York State Veterinary Diagnostic Laboratory at
Cornell
University for identification.
Since no commercially available vaccine exists against Salmonella,
disinfection and other biosecurity practices must be utilized in order
to prevent the introduction or the spread of this disease. Specific
management practices to be used are outlined in the New York State
Horse Health Assurance Program, a program designed to promote horse
health, care and welfare and to encourage horse owners to learn more
about horse management.
New arrivals and horses returning from off the farm should be isolated
from other horses so that fecal-oral spread of these organisms can be
controlled. If strict isolation is not possible, maintain closed groups
with as small a number of animals per group as possible. Since foals
seem to be most
susceptible, avoid combining mare/foal pairs with new arrivals. Shared
pastures, paddocks and stalls can all promote transmission of these
organisms
as they survive in manure, manure contaminated soils and forages, and
wet
areas. Horse trailers should be thoroughly cleaned, disinfected and
re-bedded
prior to transport of different animals. Always provide clean,
individual
food and water buckets and tubs for your horses then they are away from
home. Avoid contact with manure when visiting equine facilities, and
footwear that can be cleaned and disinfected. Do not wear the same
clothing and
shoes while visiting other horse facilities that you wear when caring
for animals at your home facility.
Environmental cleanup involves the removal of all organic material
(bedding, contaminated feed, manure), complete washing down of all
surfaces, including feed tubs, water buckets/tanks, and cleaning
utensils with water and a detergent cleaner to remove remaining organic
residues, and the
application of an appropriate disinfectant for the proper contact time.
Disinfectants used to combat Salmonella include chlorine bleach and
quaternary
ammonium compounds. Scrapers, brooms, shovels and manure forks can
spread
the organism from contaminated areas to previously uncontaminated ones.
Cleaned areas should be encouraged to dry quickly by using fans and
exposing
to sunlight, where possible. Pressure washers should be avoided, unless
all
animals have been removed and the operator wears OSHA-approved
respirator
protection, as Salmonella organisms can be aerosolized and spread this
way.
Environmental sampling can be used to determine if effective cleaning
has
been done in a facility with previously infected animals.
|